Rapid Softlithography Using 3D‐Printed Molds
Polydimethylsiloxane (PDMS) is a long‐standing material of significant interest in microfluidics due to its unique features. As such, rapid prototyping of PDMS‐based microchannels is of great interest. The most prevalent and conventional method for fabrication of PDMS‐based microchips relies on softlithography, the main drawback of which is the preparation of a master mold, which is costly and time‐consuming. To prevent the attachment of PDMS to the master mold, silanization is necessary, which can be detrimental for cellular studies. Recent advances in 3D printing have shown great promise in expediting microfabrication. Nevertheless, current 3D printing techniques are sub‐optimal for PDMS softlithography. The feasibility of producing master molds suitable for rapid softlithography is demonstrated using a newly developed 3D‐printing resin. Moreover, the utility of this technique is showcased for cell culture to show biocompatibility of the process. [...]
Please register below to read the full article digest.
Introduction
There is a growing body of literature that recognizes the significance of lithography in the fabrication of PDMS‐based microchannels. However, lithography is limited in its ability to fabricate non-straight microchannels. Therefore, research groups have tried to provide alternative methods for the fabrication of molds used in softlithography processes. One such alternative is the use of 3D printing technology for the fabrication of softlithography molds. Among all 3D printing methods, stereolithography apparatus (SLA) and digital light processing (DLP) offer great advantages, making them ideal candidates for microfluidics and biomedical applications. However, one of the limitations of 3D printed SLA/DLP master molds for softlithography is the requirement for tedious pretreatments prior to PDMS casting. Pretreatment protocols have been proposed to treat the 3D printed master mold before PDMS casting.
Four procedures are commonly used among other proposed post-printed protocols: 1) UV curing; 2) surface cleaning; 3) preheating; 4) surface silanization. Nevertheless, there is still no consensus about the optimum protocol for treating 3D printed templates for PDMS casting. In addition, the proposed protocols are time‐consuming, labor‐intensive, and lacking reproducibility. Furthermore, the treatment parameters, such as UV curing time, preheating temperature, and duration, seem to be a function of the feature size; thus, differ from one experiment to another. Also, preheating in particular is a common step in many procedures and often induces high levels of material strain, resulting in the formation of cracks within microstructures. Most importantly, surface silanization of the 3D printed templates is essential to ensure the PDMS peels off, correctly. Some silanizing agents such as perfluorooctyl triethoxysilane are cytotoxic and are not suitable for biological applications. Thus, development of a resin suitable for master mold fabrication will reduce all these time‐consuming steps.
To address the aforementioned issues, herein, the use of a new resin developed by Creative CADworks (CCW Master Mold for PDMS devices) for the fabrication of master molds directly by the DLP 3D printing method is optimized. It is shown that the 3D printed templates obtained using this resin can be immediately casted with PDMS without any pretreatment or surface modification. By way of explanation, the process of master mold design to microchip fabrication has been reduced from a time frame of several days (for a conventional softlithography process) to less than 5 h. In order to showcase the functionality of this resin, four different microfluidic devices have been developed. In this digest version, the focus lies on the application in cell culturing. The surface of the PDMS replica obtained from the 3D printed mold is also evaluated to investigate the bonding quality of PDMS.
Methods
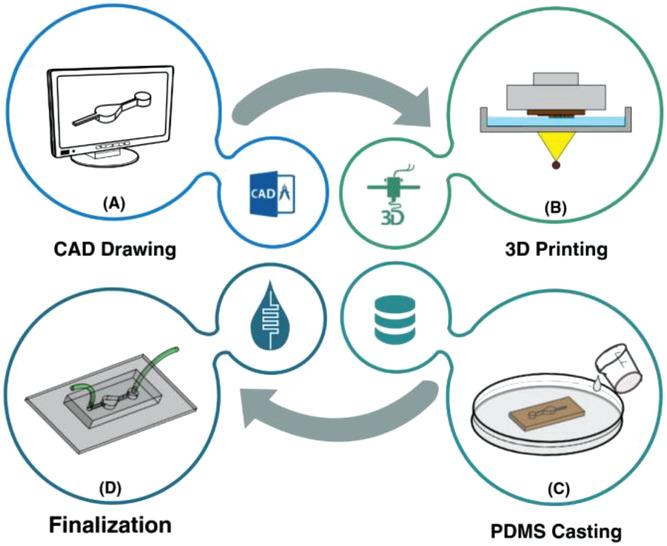
The workflow of the master mold preparation by DLP/SLA 3D printing method and microfluidic resin is shown in Figure 1. A) The desired master mold is drawn. The beauty of microfluidic devices is that they require neither intricate geometries nor professional CAD drawer. Thus, the CAD drawing process will not take a long time. B) The design is then printed using a DLP/SLA 3D printer, and the residuals are removed from the surface of the mold. C) Afterward, PDMS is poured in the master mold, and D) in the final stage, PDMS is peeled‐off, bonded to a glass or PDMS layer, and the finalization followed by the installation of inlets and outlets.
Surface characterizations of the 3D printed mold and PDMS were analyzed using 3D laser microscopy (Olympus LEXT OLS5000); to this end, an LMPLFLN 20× LEXT objective lens (Olympus) was selected. Arithmetic mean deviation (Ra), the arithmetic mean of absolute ordinate Z (x,y) documented along a sampling length, and arithmetical mean height (Sa), the arithmetic mean of the absolute ordinate Z (x,y) documented along an evaluation area were chosen to evaluate the surface characterization of the samples.
Results
PDMS Characterization
After fabricating the 3D printed molds and removal of any residual resin, PDMS was casted on the master molds. For the sake of comparison, two different molds were fabricated, one with a conventional DLP resin and the other with the newly developed microfluidic resin. The main challenge with conventional DLP resin is that due to the presence of unreacted monomers, complete polymerization of PDMS cannot occur, resulting in the presence of residual material on both the PDMS and the mold. The comparison between the mold fabricated via conventional resin and the microfluidic resin reveals that these two molds have identical surface roughness, and the smallest channel height for the fabrication of molds can be achieved with a thickness layer of 30 µm. However, for this thickness layer, the curing time of each layer for the newly developed resin is 6.5 s, which is more than the conventional one which is 1.3–1.5 s; as more time must be devoted to the methacrylated resins to be completely polymerized and cured. All in all, the fabrication time for both molds took less than an hour which is much faster than other methods. Also, the inset in Figure 2A shows the contact angle of the 3D printed molds. The contact angle measurement reveals that both surfaces are hydrophilic; however, the microfluidic resin is slightly more hydrophilic than the conventional one.
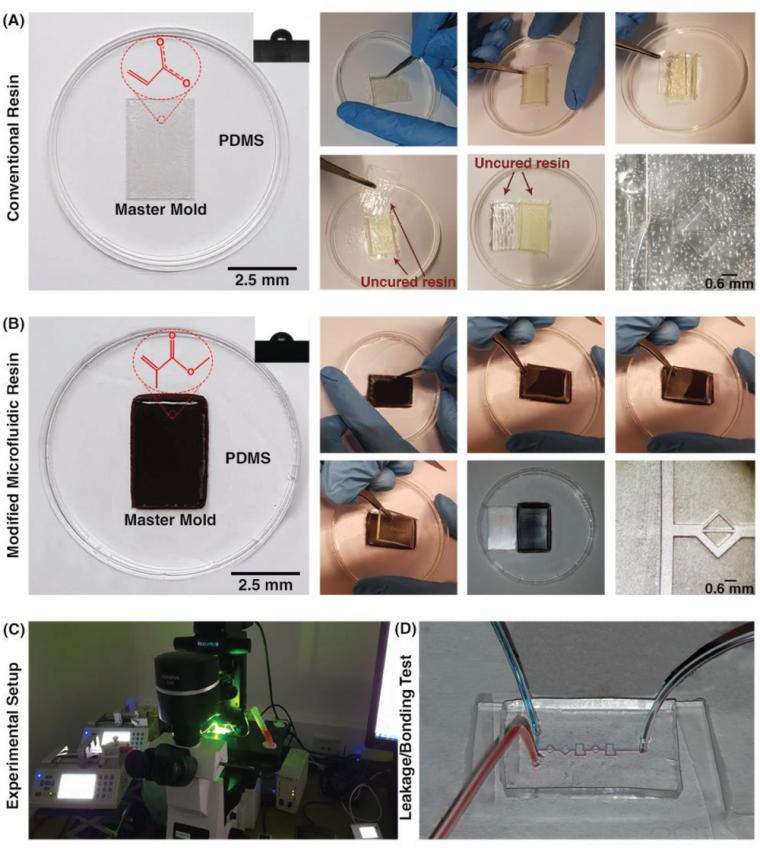
As Figure 2A indicates, in the conventional DLP resin, PDMS surfaces in contact with the surface of the resin were not properly cured, and uncured PDMS layers remained on both surfaces. It can be clearly seen that the casted PDMS fails to adopt the pattern of the mold, thoroughly. In addition, during the detachment of PDMS from the mold, PDMS tends to stick to the resin, confirming that the surface of the conventional DLP resin is not appropriate for PDMS casting. By analyzing the materials constituting the conventional DLP resin, it is believed that this problem is related to the chemical composition of the resin. We hypothesized that the remaining catalyst and monomers on the surface of the printed mold disrupt the complete polymerization of a thin layer of PDMS in contact with the mold. This can be clearly seen upon the removal of the PDMS replica from the mold (Figure 2A). As such, the “acrylate group” in the resin's chemistry is not a suitable choice for PDMS casting; this has urged different scientists to explore time‐consuming strategies for the surface treatment of DLP printed molds. Through extensive research conducted by Creative CADworks, a new resin which contains methacrylated monomers and oligomers has been developed. Casted PDMS does not react with the methacrylated monomers because the surface of the mold is free of residual monomer units that may impede PDMS polymerization. As Figure 2B illustrates, once a blade cuts through the PDMS layer down to the mold, the PDMS replica detaches easily. The operation of each device and the quality of bonding were also analyzed for a wide range of flow rates (to check the simulations results of surface roughness and bonding quality, see Section 2.2) with the experimental setup shown in Figure 2C. The results, as shown in Figure 2D, confirmed that there was no leakage observed between flow rates ranging from 0.1 to 5 mL min−1, which indicates that the proposed method for fabricating PDMS‐based microdevice is an ideal candidate for a variety of applications.
Biological Applications
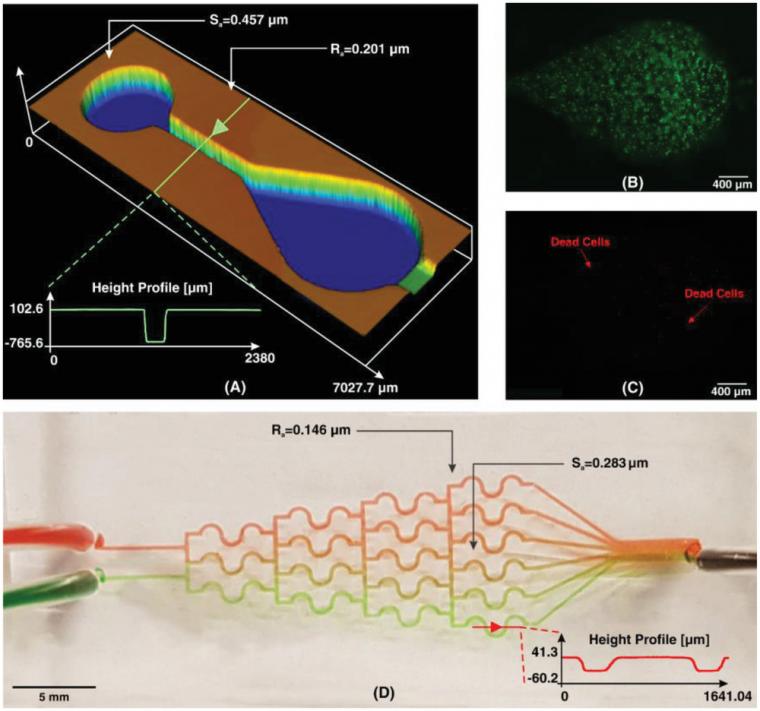
To fabricate the arrays of the microchambers, Liu et al. used standard dry etching on a silicon substrate followed by PDMS softlithography. The dimensions and characteristics of the 3D printed microchamber are shown in Figure 3A. The total printing time starting from the initial design to the final product took only 45 min. MCF‐7 cells with a concentration of 106 cells mL−1 in culture media (Roswell Park Memorial Institute (RPMI) 1640 with 10% fetal bovine serum (FBS) and 1% streptomycin–penicillin) were introduced into PDMS microchamber. The device was incubated for 24 h at 37 °C with 5% CO2. To evaluate the cell viability in the PDMS microchamber, live/dead cell double staining was performed. As shown in Figure 3B,C, more than 98% of the cells remained viable in the microchamber 24 h after the initial cell seeding. This confirms that no cytotoxic residual material had been left on the PDMS from casting on the 3D printed resin. Also, in cell culture platforms, flow rates exist in the order of µL min−1,43 and the values of Ra and Sa, as shown in Figure 3A, indicate that the device is functional within its flow regime. Therefore, it can be concluded that the newly developed resin for 3D printing master molds is suitable for cell culture applications and does not compromise cellular viability. Currently, lung‐on‐a‐chip studies using 3D printed microfluidic resin molds are under investigation in our group; these studies demonstrate long‐term cell viability (more than a week).
Discussion
The gradient of biomolecules plays a crucial in controlling various biological activities, including cell proliferation, wound healing, and immune response. One of the most popular types of CGGs that produces discontinuous concentrations is the tree‐like CGG. This type of CGG is based on the fact that one can divide and mix the flow through bifurcations and pressure differences downstream. This type of CGG is usually used for cancer cell cultures, as these CGGs transfer more oxygen and nutrients to cells as they develop a convective mass flux. Among various tree‐like CGGs proposed in the literature, we chose the S‐shaped CGG design developed by Hu et al. The authors used micromilling to fabricate the CGG on a polymethylmethacrylate substrate. Here, we developed the same structure in PDMS using softlithography based master mold fabrication from our new microfluidic resin. The device has two inlets and six outlets to produce six different concentration ranges. To examine the performance of the device, we used two colors of food dyes (please refer to the Supporting Information for dye preparation protocol). The concentration profile of the fabricated CGG is illustrated in Figure 5D, which is similar to those reported by the literature. Since the velocity in CGG devices is small,45 surface roughness cannot impose problems on the binding of PDMS. For printing of planar structures, 3D printing can be performed with higher slice thickness, as a result of which, printing time will be reduced.
In summary, the microfluidic resin for 3D printing is an ideal candidate for fabricating different bio‐microfluidic devices and can replace all cost‐intensive and time‐consuming fabrication methods.
Conclusion
In this study, we introduced a microfluidic resin for direct fabrication of master molds for PDMS softlithography, which can substitute other time‐consuming master mold fabrication methods. In the proposed master mold microfluidic resin, methacrylated monomers and oligomers have been used to facilitate PDMS casting, the proof of which was illustrated by fabrication of a cell culture device (and three other benchmark microfluidic devices as described in the full article) It was shown that the surface roughness has to be small enough so as to not create extra shear stress endangering PDMS bonding. In the conventional softlithography process, silanization is necessary to prevent the attachment of PDMS to the master mold, which can be detrimental for cellular studies. The 3D printed mold obtained from the microfluidic resin proposed here does not require any silanization, and the cellular studies in the PDMS‐based cell culture device confirmed the biocompatibility of the resin. As PDMS‐based microchannels are ubiquitous in microfluidic devices, the present study can be considered as a milestone in the microfluidic field which can reduce the brainstorming‐to‐production from a time frame of several days (including the time required for conventional master mold fabrication and post‐treatment) to less than 5 h (with the new proposed microfluidic resin).
Source: Preview Image: Mihail/stock.adobe.com